About Us
The Childhood and Adolescent Cancer and Blood Diseases Center at Maria Fareri Children’s Hospital, a member of the Westchester Medical Center Health Network (WMCHealth), is an internationally-recognized, multidisciplinary diagnostic treatment and research center extending comprehensive, quality care while leading breakthrough research in cancer and blood diseases.
Our Mission
The Pediatric Hematology, Oncology, and Stem Cell Transplantation care and research teams at Maria Fareri Children's Hospital provide innovative therapies for childhood cancer and blood disorders. Our dedicated mission includes:
- Providing state-of-the-art and personalized, quality care for pediatric patients
-
Developing innovative preventive, diagnostic, and therapeutic strategies
- Conducting scholarly clinical, translational, and basic science research
-
Implementing translational therapy that incorporates cellular, gene, and regenerative therapeutics, targeted therapy, and personalized curative strategies
- Promoting psychosocial well-being and long-term survivorship
- Educating and mentoring future generations of bright and caring health care professionals in the diagnosis and treatment of children and adolescents with cancer, blood and genetic illnesses.
Personalized Care You Can Trust
Twenty-first century treatment for our youngest cancer and blood disease patients means a personalized, targeted approach that’s both focused and gentle—one that reduces toxicity and uses groundbreaking methods to treat cancerous tissues and blood diseases. Under the direction of Mitchell Cairo, MD, Division Chief, Pediatric Hematology, Oncology and Stem Cell Transplantation at Maria Fareri Children's Hospital, our team draws upon expertise in pediatric hematology, oncology, stem cell transplantation, surgery, pathology, genetics, radiation oncology and immunology to personalize this approach for each child.
We specialize in diagnosing, treating, and researching solid tumors, brain tumors, childhood leukemias, bone marrow failure, immunodeficiencies, sickle cell disease, bleeding disorders, clotting disorders, and other hematological illnesses. View a full list of our clinical and therapeutic programs.
Cutting-Edge Research
Each day, we gain expertise, build resources and achieve breakthroughs in the treatment of cancer and blood disease. From bone marrow transplantation to stem cell immunotherapy, targeted therapy, and gene therapy, we are unlocking treatments and blazing trails to pinpoint the cause, course of personalized treatment, and cure.
Our investigations are basic, translational, and clinical—meaning that breakthroughs in the laboratory translate directly into patient care. By taking the lead in several trials investigating targeted antibodies, cellular therapy and stem cell transplants, the Center has immediate access to pioneering research that informs therapeutic strategies and enhances quality of care.
Putting Our Patients First
We know, as you do, that each child is unique, and each one deserves the science-based medicine and the holistic support to sustain him or her—in body, mind, and spirit—through the challenges of sickness. From the bedside to behind the scenes, our approaches center on our patients, and from the minute you arrive at the hospital, we’re in this together.
Active family involvement creates the environment that allows us to provide advanced care, especially through the physical and emotional rigors of prolonged illness. Children in treatment for cancer or blood disorders at Maria Fareri Children’s Hospital may stay here for an extended period of time, but they will never feel “hospitalized.” Instead, they will engage with their families, peers, care providers, and others on their journey toward healing.
Our Supporters .png)
We are sincerely grateful to all of our supporters. A special thank you to our major supporter, the Pediatric Cancer Research Foundation,
for 41 years of continuous and dedicated funding to our PCRF Laboratory.
- The Children’s Cancer Fund
- Dystrophic Epidermolysis Bullosa Research Association
- Food and Drug Administration
- Hyundai Hope On Wheels
- Maria Fareri Children’s Hospital
- Westchester Medical Center
- Department of Defense
- National Institutes of Health
- New York Medical College
- Paul Luisi Foundation
- Pediatric Cancer Foundation
- St. Baldrick’s Foundation
- The Gardner Marks Foundation
- Marisa Fund
- The National Cancer Institute
- Alex's Lemonade Stand Fund for Childhood Cancer
If you would like to learn more about how you can support our mission to save the lives of children, then please contact our administrative office at 914.594.2150.
Our Heroes
Meet Some of Our Heroes
Althea Salmon
Today, you can speak with Althea Salmon and have almost no hint of what this strong-willed fourteen-year old has spent her life battling. Born in 1999, Althea was diagnosed during newborn screening with Sickle Cell Disease, a hereditary blood disorder effecting hemoglobin that can impact nearly every organ in the body. It brings on a host of severe health issues including the potential for acute life threatening complications of the lungs, brain, and immune system, as well as severe anemia. Patients also suffer from recurrent and severe episodes of pain that are debilitating and require strong doses of pain medications. Already having a son diagnosed with the disease, Althea’s mother, Joan, knew that it would likely mean a life in and out of hospitals for her daughter. For Althea, this would be the least of it.
One morning, while helping her daughter dress for school, Joan noticed that Althea was only using hand. It had turned out that at the tender age of only four years, Althea had suffered her first stroke, impairing her hand. Joan recalls that nothing ever kept Althea down, even at such a young age, she was a strong girl with determination.
Nevertheless, suffering from strokes brought on further complications within Althea’s brain known as the Moyamoya syndrome. In 2006 and again in 2009, Althea would need brain surgery in an effort to alleviate some of the chronic changes brought on by Moyamoya. At this point, because Althea was a high risk candidate for continued strokes and permanent neurological damage, it was imperative to consider other avenues of support and treatment.
Althea’s mom came to find out about Dr. Cairo and a novel treatment strategy he is pursuing for Sickle Cell Disease in pediatric patients. While stem cell transplants are the only curative option for Sickle Cell Disease, most of the success in curing the disease has been limited to matched sibling stem cell transplants. Statistically, most patients with Sickle Cell Disease do not have a matched sibling donor, therefore the need to develop effective alternative options for performing a curative stem cell transplant in these patients has been dire, especially for patients like Althea. By using the stem cells of a parent, or a related haplo-identical blood stem cell donor, Dr. Cairo has been able to provide the hope for a cure for the vast majority of patients suffering from Sickle Cell Disease. After meeting with Dr. Cairo and weighing their options, Joan and Althea decided to move forward with the transplant. While Althea admits that perhaps she was a little nervous and thought it might be scary, her reaction was “Let’s do it!” For Joan, there was no other real option for her daughter.
Althea would undergo both chemotherapy and radiation prior to the transplant. Besides losing her hair, dealing with mucositis and nausea, Joan saw her daughter pushing and fighting for strength and a chance for a normal life. Joan recalls telling Althea over the years: “never let sickness get the better of you.” And certainly, Althea has not.
Althea is now cured of her sickle cell disease with no more symptoms related to the disease.
Meet More Heroes
Nick Scianna 
As he had done countless times before, 15 year old, Nick Scianna headed off to his high school basketball practice unaware of how his life was about to change. A typical teenager, high school basketball and baseball player, and active in both his church and community, Nick was about to face the toughest game of his life.
During practice Nick became injured and needed to be transported by ambulance to his local area hospital with a bruise the size of a cantaloupe and horrific pain on the left side of his abdomen. At first, the doctor thought that he had broken a rib, or at worst, ruptured his spleen. However, an X-ray would show his ribs to be fine, and CT Scan taken would reveal nothing other than an enlarged spleen. Unfortunately, further blood work and other tests taken that afternoon would suggest that something more serious was going on. Nick needed to be transported that evening to Maria Fareri Children’s Hospital and admitted into the Pediatric Intensive Care Unit where specialists could better understand what was happening.
Over the next few days many tests would be performed by various specialists, but gave no clear answers. Finally after 3 days in the Pediatric ICU, the Pediatric Hematology/Oncology Doctors would perform the tests that would bring to light what was happening to Nick. A bone marrow biopsy would reveal that Nick had “High Risk B Acute Lymphoblastic Leukemia,” otherwise known as “A-L-L.”
The “Arts Unit” at The Maria Fareri Children’s Hospital would now become Nick’s “home away from home” as treatment began promptly after diagnosis. Sadly, by early spring of 2011 it was very clear that Nick’s cancer was tougher to get into remission then most ALL patients. A more intense chemotherapy regimen still did not yield the results hoped for. Under the guidance of Dr. Mitchell Cairo and the hematology oncology team, it was decided that Nick’s only option for survival and possible long-term remission would be a Bone Marrow Transplant.
On the morning of May 27, 2011, Nick received a transplant from a completely unknown donor found on of the National Bone Marrow Registry. The transplant process and recovery has been a very long and hard uphill battle for Nick. He has overcome a multitude of complications from his transplant and thankfully remains in remission.
With all of this, the hardest thing for Nick is his desire to just live a normal life. There’s nothing typical about going through a battle like this. In the fall of 2014, Nick began his first semester at Mt. Saint Mary’s College on a full scholarship for the 5-year MBA program. Although he continues to deal with effects of the treatment on his kidneys as well as GVHD, Nick has drawn strength from his faith and those around him, especially his mother. He has kept his eye on the ball during these hard times and is excited to continue moving forward with his life.
Meet More Heroes
Peter Pinori 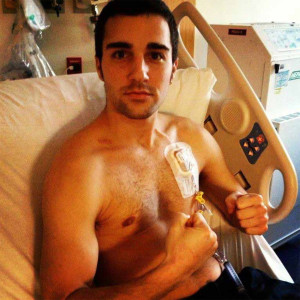
“God gives the toughest battles to his strongest soldiers.” Meet one of them: Peter Pinori.
In December 2012, 24 year old Peter, woke up to find a small lump in his neck. His primary doctor sent him to an ENT, where they ordered a needle biopsy of the lump. But by this time, the lump seemed irrelevant because he had developed another lump; this one was the size of a golf ball.
On December 14, 2012, Peter was diagnosed with Stage 4 Hodgkin’s Lymphoma which means it had metastasized to his neck, spine and abdomen. After his diagnosis, he was transferred to Maria Fareri Children’s Hospital on a recommendation from his sister Daniela. Daniela works as a Pediatric Oncology Nurse and recommended that he be seen by Dr. Mitchell Cairo. After he had a phone conversation with Dr. Cairo, Peter told his family: “I had a good feeling about the whole thing.”
Peter recalls: “I took the news better than my family. Cancer takes a big hit on your life. When I found I had cancer I was like ‘really?’…and finding out I had Stage 4 Cancer was a devastating blow.” But that didn’t change his spirit, “you have to remain positive. Stay funny, keep people close to you happy. My family was strong and kept me going.”
Following his second round of chemotherapy, the doctors ordered a PET scan, as they routinely do, in order to see if the chemotherapy is effective in treating the cancer cells. When they returned to tell him the results, they told him there was no trace of disease. In other words, the therapy had worked and he was in a complete remission and cancer free!
After six months of chemotherapy, Peter feels he is lucky to be here. “Six months of chemotherapy to some of these kids is nothing. They have been through so much more, I’m the lucky one.” He also credits the Doctors, Nurses and Staff at Maria Fareri Children’s Hospital to his healthy return. “This place is amazing. The care and hospitality here are the best in the world. The doctors and nurses are like family to me.” Peter would like to help other kids in the future that are going through the same experience. “I’d like to talk to kids to help them what they are going through.”
The whole experience gave Peter a new perspective on life. “Going through cancer, you have no excuse to complain about anything. Life can’t be that bad anymore. I want to keep living and want to enjoy my life.” Peter is inspired to try out for the American Ninja Warriors – where hundreds of competitors challenge themselves against an obstacle course to qualify for a shot at making it to Japan to compete in Sasuke 23. The prize to win is a half million dollars which he plans to donate if he wins.
“Having cancer is like going through an obstacle course. If this didn’t beat me, nothing can.”
Meet More Heroes
Ryan Gilchrist 
Meet Ryan Gilchrist or better known by his friends “Gilly”. Going into 8th grade, he was an avid sports player; hockey, lacrosse, basketball, you name it. In January of this year, he started experiencing stomach pains. They kept getting worse over time, to the point that during midterms at school, he had to check himself out and into a hospital to find out what was wrong.
On January 23, Doctors at Maria Fareri Children’s Hospital discovered that he had Non-Hodgkin’s B-Cell Lymphoma. “I was shocked and a little scared. I didn’t know what to expect. But the support from my friends and family was incredible.” Ryan’s cousins initiated “Team Gilly” to show support during his battle with Non-Hodgkin’s Lymphoma. Ryan’s friends, classmates and teammates were all active participants in his fight against Cancer under one united “Team Gilly”.
As the Gilchrist family did their due diligence on where to go and how to treat their son, they reached out to their community including friends, family, and co-workers for advice. In an almost unanimous decision, all arrows pointed to a world-renowned oncologist and expert on B-cell lymphoma at Maria Fareri Children’s Hospital, Dr. Mitchell Cairo. When all was said and done, Ryan started chemotherapy and was completely cancer free in 90 days. “We had a party when the last bag of chemo was finished. It was a great feeling to be done.”
Ryan says he is humbled by his experience and hopes to help out other kids that are going through the similar struggle he went through. We have come a long way to treat lymphoma and Ryan can attest to benefitting from a more effective, less toxic therapy and shorter treatment period. This allowed him to return back to a normal life and to the sports that he loves. Ryan is just one of many amazing examples of the research being done by PCRF and the lives that your support and contribution are saving.
Meet More Heroes
Hanif Mouehla 
Despite both of Hanif’s parents, Khuraira and Patrice, being carriers of the Sickle Cell trait, they were confident that he would not be born with Sickle Cell Disease. Already having had 2 children without the disease, Hanif’s parents felt that he would be no exception. Hanif’s vibrancy as a newborn made Khuraira all the more certain. However, results from testing after his birth proved otherwise. Having lost friends and family from Sickle Cell Disease, Khuraira and Patrice were devastated by the news. However, they pledged to be optimistic for their son’s future. Having come to the United States from Nigeria, they knew the quality of care would be better for their son than their friends and family had experienced. Despite this, Hanif and his parents would be severely tested by the disease.
Hanif’s worst crisis came just after his eighth birthday and landed him in the hospital on a ventilator for acute chest syndrome. The attack grew so severe that he had to be transferred by ambulance to the Intensive Care Unit of Maria Fareri Children’s Hospital. Hanif’s condition continued to worsen and doctors had no choice but to place him in an induced coma after both of his lungs collapsed. He was induced for six weeks and doctors were uncertain if he would make it. His parents were in tremendous turmoil with limited options that could help their son. It was during this time that a physician from the Division of Pediatric Hematology Oncology and Bone Marrow Transplant came to visit Khuraira and Patrice to let them know that a bone marrow transplant from a mother or father would be an option for Hanif if he survived this crisis. Luckily, Hanif pulled through but his functioning was impaired.
Upon his recovery, Khuraira and Patrice considered bone marrow transplantation as the only way to save Hanif from another life threatening crisis. Unfortunately, he had no tissue matching sibling donors. After meeting with Dr. Cairo and other physicians in the division, his parents were worried about associated risks, but decided that given Hanif’s pattern of crisis, a transplant would give him a better chance for life. Hanif underwent a familial haploidentical stem cell transplant from his mother as the donor on the research protocol. Today, Khuraira and Patrice are confident they made the right decision for their son. Currently, Hanif is one year out from his transplant and is sickle cell disease free and without pain, and has resumed a normal life. He wants to a write a book to share his experience with other kids and cannot wait to be old enough to become Dr. Cairo’s assistant! His ultimate goal is to be a doctor so he can help find a cure for Sickle Cell Disease so that no child has to go through the pain he endured.
Meet More Heroes
Sean Cadden 
Found by chance after he broke a tooth on the playground, Sean was diagnosed on November 22, 2010 with Acute Lymphoblastic Leukemia (ALL). The next three and a half years were followed by medication, chemotherapy, lumbar punctures and bone marrow biopsies. In May 2014, Sean got the “all clear” from the doctors and his medical port was removed.
That August, Sean’s family planned a two-week beach vacation to celebrate. Upon returning from vacation, Sean complained of pain in his legs and feet. After a visit to the podiatrist and testing for Lymes disease and mono came up negative, a bone marrow biopsy was done to “rule out” a relapse. Sean’s family’s worst fears came true when the test came back positive for cancer.
Treatment for this type of relapse is a stem cell transplant or bone marrow transplant. Sean initially spent four weeks in the hospital from August to September undergoing high dose chemotherapy and three separate surgeries. Then the search for a stem cell donor began. The first step was to test Mom, Dad and his sister, Marijane. The doctors were not optimistic for a related match and suggested sending Sean’s needs to the National Bone Marrow Registry. Finally, a glimmer of hope appeared as Sean’s sister Marijane (MJ) was identified as a perfect ten-point match. For understandable reasons, MJ was scared. She endured repeated blood work and painful pre-medications in order to prepare for the harvest.
On November 1, 2014, Sean was admitted to the hospital to prepare for his transplant. He underwent seven days of more chemotherapy and an additional five days of radiation; Sean had never received radiation before. On November 13, Sean’s Birthday, MJ was admitted for her big donation. Two doctors drew her marrow and Sean received that marrow the next day.
In total, Sean spent eleven and half weeks recovering in the hospital. He was released on Jan 21, 2015. He still has a long road ahead of him including twice weekly trips to the doctor and home medications including daily IV’s. Dr. Cairo and his team of doctors and nurses keep a close eye on him and on all accounts he is doing very well.
Meet More Heroes
Gabriel Sanchez
On December 25, 2001, we welcomed our angel Gabriel into this world. Christmas for us has never been the same….a true blessing! The last 10 years have been difficult, an emotional roller coaster to say the least, but we are still blessed. Starting from the age of just six months old, Gabriel had a host of medical issues including cradle crap and severe allergies on this earlobes, nose and lips. This made life for him very difficult as a baby.
In January 2005, at the age 3, Gabriel began to have a severe case of bloody diarrhea that did not resolve with antibiotic treatment. At our very first appointment the doctor reviewed the labs immediately sent us straight to the emergency room. I remember that sinking feeling and I just cried while the doctor told us she wasn’t sure what was wrong. I remember Gabriel, who had just started putting sentences together, saying, “Mommy, please don’t cry” over and over. For about 3 weeks no one could tell us what was wrong with our baby. Why was he so sick? Eventually, he was diagnosed with Crohn’s and put on what we were told would be his lifetime medication. In September of the same year, while still suffering from bloody diarrhea, Gabriel developed an abscess on his neck that needed to be drained. While the abscesses were somewhat controlled with antibiotics, they would continue for years. In addition to the abscesses, Gabriel had always presented with skin problems such as severe crusting around his nasal passages that would blister and bleed, blisters on his lips, mouth sores. Needless to say this caused Gabriel to feel bad about going to school for fear of being made fun of. We did everything to keep him healthy….we just didn’t know there was anything different that we could have done to make it better.
We’ll call it motherly instinct, but I still was not convinced that Gabriel had Crohn’s and in 2008, without telling the doctor, I took Gabriel off his “lifetime” antibiotics. In August 2011 Gabriel’s gastroenterologist was very surprised that he had not relapsed and did more testing that finally ruled out Crohn’s disease.
Unfortunately, our happiness did not last too long. On September 29th we had to bring Gabriel into the emergency room due to fevers above 100 degrees lasting for 2 weeks. At the emergency room a CT Scan revealed that the reason for the fevers were due to 3 abscesses in the liver; and we were once again admitted.
After years of sickness, some determined doctors came to find that Gabriel was born with Chronic Granulomatous Disease (CGD). That would offer us the relief of knowing what was wrong with Gabriel, but we still needed to remove the abscesses from Gabriel’s liver. We tried every option, surgery, drains, nothing worked. The last resort would be a liver transplant. This was very scary news…too much to bear really. Just when Gabriel was ready to go down to have a liver resection, the immunologist received information on a recent study that showed 8 out of the 9 patients with liver abscesses successfully treated using corticosteroids. The study was only in the stages of being reviewed for approval and not even yet published. We agreed to treat Gabriel with the steroids. This helped Gabriel, but was not a cure. Gabriel’s immunologist and surgeon recommended that we consider a cure for the disease by way of a Bone Marrow Transplant. Fortunately, coming from the Bronx, we did not have to relocate in order to receive treatment like so many other families. We met with Dr. Cairo in January 2012 who provided with us with many options for a cure for Gabriel and put us at ease with his extensive work on CGD and Transplants. Gabriel received 7 days of reduced intensity chemotherapy and the transplant was completed on April 25th, 2012 using cord blood from an unrelated Hispanic female with 5/6 match.
Gabriel was discharged 57 days after his transplant and has been doing extremely well despite complications with his lungs for the greater part of 2013 due to a very serious infection of.
Thankfully as of June 2013, Gabriel was lifted off of all medications and IVs that were administered at home. Despite some of the complications, we received the great news that he is cured and no longer needs to be isolated to minimize risk of infections.
Today, Gabriel is slowly starting to resume a more normal life for an 11 year old boy. A life-time of medications would have caused a host of complications for him, but he is large as life and a true warrior!
Meet More Heroes
Success Stories
17-Year-Old Who Beat Life-Threatening Disease Now Hopes to Become Doctor — and Is Headed to Harvard! (People Magazine)
Sickle Cell Disease Survivor Pays It Forward (NBC4)

My Sister, My Hero

A New WMCHealth-Led Study Offers Hope to Sickle Cell Disease Patients

News
8-Year-Old Sickle Cell Ambassador (as seen on NBC New York)
VALHALLA, NY (September 29, 2021) - Hear from 8-year-old ambassador, Camryn Kellam, about how she is thriving after undergoing a successful stem cell transplant to treat Sickle Cell Disease at Maria Fareri Children’s Hospital. See her on NBC4. You’ll also hear from Dr. Mitchell Cairo, Chief of Pediatric Hematology, Oncology and Stem Cell Transplantation at Maria Fareri Children’s Hospital, about innovations in the field. (Watch more via Hudson Valley News12.)
Westchester Warriors Season Opener Raises $2,500 for CTEL at Maria Fareri Children's Hospital
YONKERS, NY (April 20, 2019) - We extend our deepest appreciation to Westchester Warriors Hockey youth players for raising $2,500 at their season opener on April 20! Contributions for the 2019 season will support the Cellular and Tissue Engineering Laboratory (CTEL) within the Children and Adolescent Cancer and Blood Disease Center at Maria Fareri Children’s Hospital. CTEL creates and provides patient-specific life-saving therapies for pediatric oncology patients.
Over 300 families and players attended the game, which featured a puck drop by Yonkers Mayor Mike Spano. ShopRite in Tuckahoe generously donated bottled water and snacks for guests. To learn more about the Westchester Warriors youth hockey players' fundraising efforts, visit http://westchester-warriors-hockey-2019.everydayhero.do/

Pictured here: Luis Panchame, Westchester Warriors co-Founder; Mayor Mike Spano of Yonkers; Alex Gittleman, Director of Events for the Westchester Warriors; members of the ‘07/’08 Warriors Team. Photo courtesy of Tim Ramundo.
Maria Fareri Children's Hospital and Westchester Warriors Youth Hockey Program Unveil "Westchester Warriors Way"
VALHALLA, NY (January 15, 2019) - Maria Fareri Children’s Hospital and the Westchester Warriors Youth Hockey Program unveiled Westchester Warriors Way – a new entrance to the expanded Center for Pediatric Oncology and Cellular Therapy at Maria Fareri Children’s Hospital.
Since 2016, the Westchester Warriors Youth Hockey Program has partnered with Maria Fareri Children’s Hospital to fight children’s cancer, a mission started by Westchester Warriors Co-Founders Luis Panchame, Denis DuFresne and Ron Vitale. To date, the Westchester Warriors have raised over $230,000 for Maria Fareri Children’s Hospital, and the club’s efforts will continue throughout the year.
Scroll Down for Photos

Pictured, from left, Michael Gewitz, MD, William Russell McCurdy Physician-in-Chief at Maria Fareri Children’s Hospital (back row left), Michael Israel, President and CEO, Westchester Medical Center Health Network (second left) and Mitchell Cairo, MD, Chief of Pediatric Hematology, Oncology & Stem Cell Transplantation at Maria Fareri Children’s Hospital (second row center) join Westchester Warriors Youth Hockey Club Co-Founders Luis Panchame (back row center), Ron Vitale (second right) and Denis Dufresne (far right) help Westchester Warriors Youth Hockey Club players and fans celebrate the opening of Westchester Warriors Way at Maria Fareri Children’s Hospital.

Westchester Warriors Youth Hockey Club Co-Founders Luis Panchame (left), Denis Dufresne and Ron Vitale in front of the plaque commemorating Westchester Warriors Way at Maria Fareri Children’s Hospital.

Mitchell Cairo, MD, Chief of Pediatric Hematology, Oncology & Stem Cell Transplantation at Maria Fareri Children’s Hospital reveals the plaque commemorating the opening of Westchester Warriors Way at Maria Fareri Children’s Hospital. Looking on are Michael Israel, President and CEO, Westchester Medical Center Health Network (left) and Westchester Warriors Youth Hockey Club Co-Founder Luis Panchame.
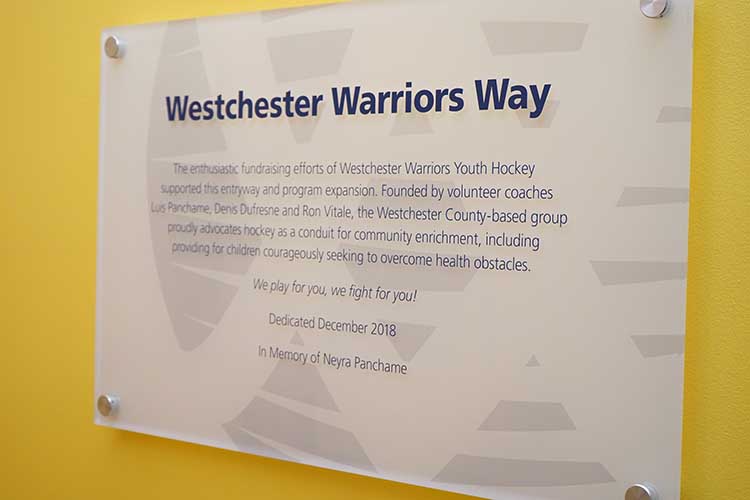
Commemorative plaque adorns the wall outside of Westchester Warriors Way, a new entry point for children and families entering Center for Pediatric Oncology and Cellular Therapy at Maria Fareri Children’s Hospital.

Westchester Warriors Youth Hockey Club jersey’s share the club’s mission and message.

Dozens of players, families and hospital representatives attended the dedication ceremony for Westchester Warriors Way.